1. Introduction
“Unprecedented global forces
are shaping the health and well-being of the largest generation
of 10- to 24-year olds in human history. Population mobility, global
communications, economic development and the sustainability of ecosystems
are setting the future course for this generation and, in turn,
mankind. At the same time we have come to new understandings of
adolescence as a critical phase in life for achieving human potential.”
The Lancet Commission on Adolescent
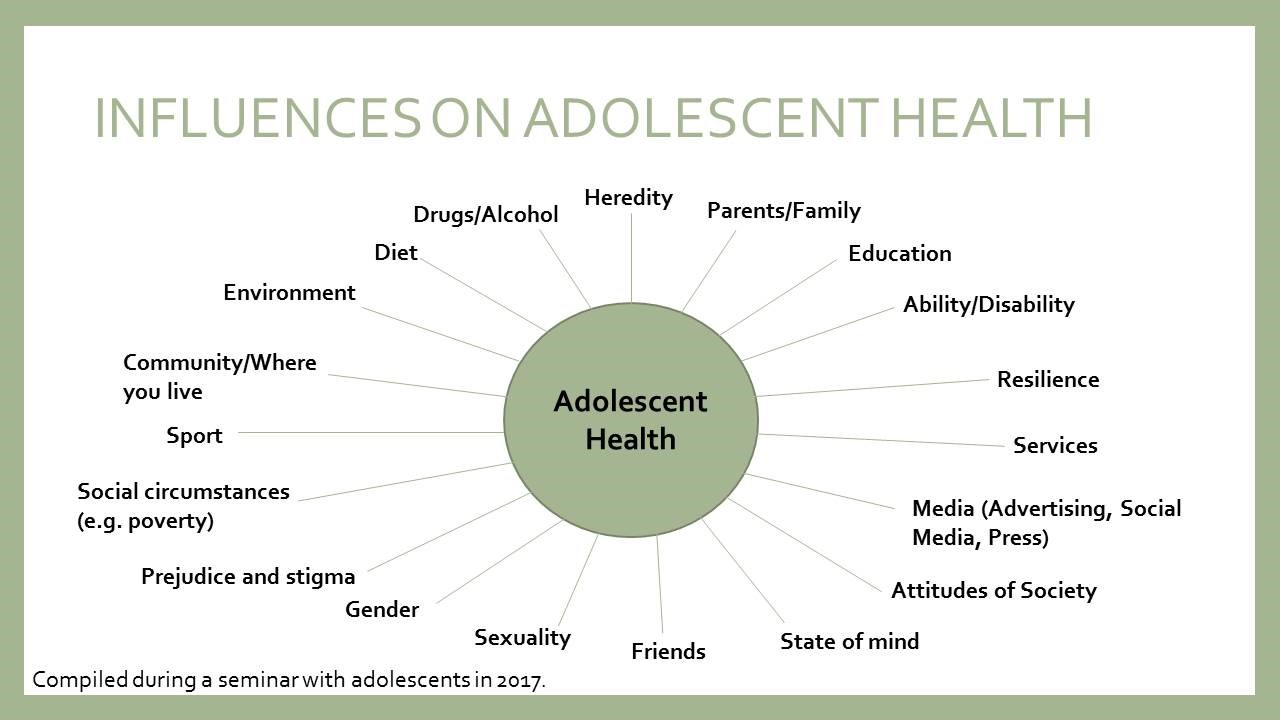
Health and Wellbeing” 
1. Adolescents can be challenging.
They are sometimes demonised and medicalised in relation to “problems”.
Adolescents can also be enthusiastic, energetic and passionate about
issues relevant to their own concerns such as education and health
and to the future of the world such as poverty, climate change and migration.
Adolescents are generally healthy, but there are sufficient numbers
who have problems to merit an increased focus on research and interventions.
Adolescence is a time in which positive changes can be made and
difficulties addressed and resolved. We must take better account
of the potential of adolescence for achieving human potential, for
the benefit of the whole society.
2. The United Nations Committee on the Rights of the Child (UNCRC)
notes that achieving the right to health is dependent on the realisation
of many other rights, such as those inherent in social determinants
– the conditions in which people are born and live.

The
World Health Organization (WHO) produced as long ago as 1993 a report
on the health of adolescents

and has continued to publish statements
and guidance. The United Nations Children's Emergency Fund (UNICEF)
has published a draft “Young People’s Agenda” for consultation.
It calls for a response to the Sustainable Development Goals (SDGs)
by involving leaders from governments, private sector, civil society
and youth organisations in delivering change in protecting and empowering
adolescents through education, health, skills and training.

3. This report takes up some of the global implications raised
by the Lancet Commission

and by international
organisations. Five key principles underpin its content: 1) adolescence
is a key stage of life and merits attention and investment; 2) young
people should participate in developing strategies which affect
their health; 3) welfare and other services should be co-ordinated
in a holistic way; 4) inequalities seriously undermine health and
must be addressed in order to prevent poor outcomes; 5) international
strategies for action need to be implemented at national, regional
and local levels and success or failure evaluated. These principles
will be reinforced in the sections related to mental health, sexual
health and obesity. The report seeks to present a brief overview,
a “snapshot” of factors influencing the health of adolescents and
what may be done in order to improve their lives and involve them
in doing so. It is based on selected research and the experiences
of young people, researchers and practitioners, and draws conclusions
on how the nations of Europe might develop and implement health
strategies which serve all adolescents, irrespective of their backgrounds.
A study visit to Sweden provided examples of challenges and good
practice (for further information, see document
AS/Soc/Inf
(2019) 01 on the website of the Committee on Social Affairs, Health
and Sustainable Development).
2. Adolescence is a key stage of life
which merits attention and investment
2.1. Defining
adolescence
4. For the purposes of this report,
the WHO definition is adopted: an adolescent is a person between
the ages of 10 and 19; young people are individuals between the
ages of 10 and 24. A child is someone between the ages of 0 and
18.
5. Adolescence is a unique phase of life in that it is one of
biological development, social experiences and identity building.
In particular, the impact of hormonal changes and an increased emphasis
on relationships and sexuality can make life complex for adolescents.
Added to this, the digital age and social media, whilst offering
opportunities for learning and interaction, also pose problems of
the potential exploitation of young people, including sexual exploitation.
Facebook and Google have been urged to take more responsibility
for the pressures they place on young people.
2.2. The
life course approach
6. Delivering health services
for adolescents is more than focusing on individual aspects of health,
such as smoking, drug use, diet, mental health and sexual health
at a specific age. Young children become adolescents, who in turn
become adults and grow old. Over this period, health needs will
change and a life course approach to health is required. Such an
approach aims to introduce or reinforce interventions throughout
life. It includes a healthy start to life and addresses the needs
of people, with their participation, at all stages. It addresses
the causes of ill health and promotes timely investment and a good
return for money spent. For example, education about relationships
and sexuality is delivered from different sources, before the onset
of sexual relations. In schools a “spiral” curriculum can be developed
which introduces and repeats concepts such as friendship as the
child matures. This can lead on to discussions about contraception,
sexually transmitted infections and sexual relationships at later
stages.
7. Recent research indicates that the influence of brain development,
within physical and hormonal changes and social and environmental
influences, contributes greatly to adolescent health outcomes. The Welcome
Trust has an extensive programme of research on the teenage brain
entitled “Neuroscience and Education”.

In 2017, the UNICEF office of research
(Innocenti) produced a compendium of articles under the title: “Adolescent
Brain Development: a Second Window of Opportunity”. They include:
the developing brain in its cultural contexts; poverty and the adolescent
brain; helping teenagers develop resilience; mindfulness mediation
and its impact; and the perils and the promise of technology for
the adolescent brain.

2.3. Characteristics
of adolescent health
8. According to the United Nations
World Population Prospects revision of 2015, the proportion of the adolescent
population in countries of Europe is 14%.

The number
of adolescents has grown as a result of prevention and intervention
focused on childhood health problems such as malnutrition, infant
mortality and infectious diseases. Whilst in some countries these
concerns still exist, what we are now seeing is a rise in concerns
about mental health, obesity and sexual health.
9. Adolescents are not a homogeneous group and the concept of
health cannot be separated from the context in which it exists.
Health has social determinants which influence health and well-being
status (see Diagram 1 below). Health inequalities still exist and
will profoundly affect the life chances of adolescents. WHO considers
that gender and socioeconomic differences in young people’s health
and well-being are of fundamental importance

. Some young people have greater health
risks than others, particularly those living in deprivation, those
with disabilities, those from ethnic minorities, lesbian, gay, bisexual,
transgender or intersex (LGBTI) young people and those in the youth
justice system. Young people living in zones of armed conflict are
vulnerable to exploitation and trauma.

Lack
of stability due to displacement and migration, poor education,
abuse and lack of support have powerful negative impacts and need
to be addressed in urgent ways.

Diagram 1: Influences on adolescent
health 
10. Increased emphasis on education,
especially for girls, provides greater opportunity, potential and encourages
ambition. Laws such as those on forced marriage and female genital
mutilation, whilst not always adhered to, exist to protect young
people. Other laws may restrict their rights; sexual rights, for
example, are, in some countries still limited and deny the education
and services essential to the welfare of adolescents. Whilst most
countries have ratified the United Nations Convention on the Rights
of the Child, cultural practice and national laws may lead to young
people’s rights being infringed.
2.4. Health
services for adolescents
11. Two opinions from young people
reflect the importance of having readily accessible services specifically designed
for young people. A 20-year-old woman said: “I believe promoting
more youth friendly health services is the most significant point,
as I feel there is great importance in making health care accessible
for young people.” Another stated: “Very often there is no help
available until the problem has become totally unmanageable.”

Many adolescents
are not getting the help they want when they want it. The situation
is further complicated by adolescents being on the cusp between
childhood and adulthood. They are all too frequently pushed into
services designed for adults and run by professionals without specific
training to deal with the needs of a younger age group. There is
an urgent need to improve levels of trained staff and to co-ordinate
between the different services. As one young person from an advocacy
group stated: “Young people do not want to be sent to a different
service for every different problem they are dealing with. They
want someone to help them through a variety of different issues,
recognising that they are often connected.”

12. Education for health is also important, particularly when
linked to other services. Health Promoting Schools

and
Rights Respecting Schools

exist
in small numbers across Europe. In these schools, young people learn
about their rights and health options. In addition, they may be
put into contact with professional services outside school. Health
Education, however, is rarely given mandatory status in the curriculum.
Where it exists, it is often purely biological and consists of one-off
lessons. Some schools do have programmes which not only include
information, but also encourage pupils to explore their attitudes
and values and foster decision- making skills. That said, the numbers
of school nurses and counsellors are often inadequate to cope with
young people’s health problems.

In England, after
many years of lobbying of government by politicians, professionals,
parents, young people and non-governmental organisations (NGOs),
Personal, Social and Health Education (PSHE) has been made mandatory
and includes wider aspects such as relationships and interaction
with environmental factors.

Higher
education institutions need greater support to develop health and
pastoral care systems.
2.5. Why
invest in adolescent health?
13. The 2016 Lancet Commission
considers that adolescent health has been grossly neglected.

The 2014 WHO report on adolescent
health states that adolescence is a critical time for human development
and should be given particular attention.

A 2018 World Bank report estimates
that over 90% of research publications focus on children under five.

Unarguably, the early years of human
life are important. Children deserve attention, and good access
to services,

but
so do adolescents. Attention paid solely to the under-fives may result
in national deficits of data, research, funding, policy and action
for adolescents. Focus on the early years has undoubtedly helped
with achieving the Millennium Development Goals (MDGs), but development
which occurs just before adulthood is equally important due to its
complex nature and amenability to intervention.
14. Adolescence is a dynamic and formative stage in the passage
to adulthood which can greatly contribute to satisfaction and achievement,
but can also give rise to negative experiences and difficulties.

UNICEF stresses the need to invest
in adolescence, not only because it is “right in principle” but
also because it safeguards the initial investment in health and
provides an early start for societal goals such as alleviating poverty,
achieving equity and eliminating discrimination.

Investment in health also helps to
equip adolescents with the necessary tools and coping skills for
present and future challenges.

The Lancet
Commission states that investment in adolescent well-being brings
a triple dividend of benefits now, in future adult life, and for
the next generation of children. Tackling preventable and treatable
adolescent health problems will bring huge social and economic benefits.
This is key to addressing health issues in all countries by 2030.

See the Appendix for further
information.
3. Mental
health
15. Research shows that most mental
health problems begin before the age of 25 and are most common between
the ages of 11 and 18.

Mental
health disorders can affect general health. For example, depression may
result in overeating and physical inactivity, with adverse consequences.
Not all problems persist into adulthood, especially if the episodes
are brief and appropriate interventions are applied, which are community based
with integration of services across health, education and social
sectors.

Public health expenditure
is relatively cost effective compared with health care expenditure.
Public Health England has estimated that the median return on investment
is 14.3 to 1.1.
16. WHO defines mental health as “a state of well-being in which
every individual realises his or her potential, can cope with the
normal stresses of life, can work productively and fruitfully and
is able to make a contribution to her or his community”.

Mental
health problems may be more or less common, may be acute or long
lasting and may vary in severity. They manifest themselves in different
ways at different ages – for example, in children they may manifest
themselves as behavioural problems.

3.1. Influences
on mental health
17. In Diagram 1 above, influences
on adolescent health are suggested, recognising that such determinants may
have their origins in childhood and may persist into adulthood (the
Life Course). Determinants of mental health may include: truancy
rates at school and lack of education, attainment in the early years,
first contacts with the justice system, being in care, domestic
abuse, suicide of family or friends and stigma (including racial, religious
and sexual orientation prejudice). In addition, students in schools
and higher education report stress and depression due to tests and
examinations. The influence of the media can be positive (for example,
in the promotion of access to services and advice), but also can
be detrimental, for example in cyberbullying, the portrayal of violence,
as well as pornography and grooming. In the United Kingdom, out
of 1 000 young people aged between 11 and 25, 47% had experienced
bullying.

18. Over one third of 15 year olds in the United Kingdom are “extreme
internet users” – that is, they spend more than six hours of a weekend
day on the internet and 94% use the internet before and after school.

This year WHO has added “gaming disorder”
to its International Classification of Diseases.

Spending too much time online can
create social isolation. It can also create sleep deprivation and
poor quality sleep, which can cause problems with concentration
and with behaviour and self-image – 38% of young people report that
social media had a negative impact on how they feel about themselves;
48% of girls stated that social media had a negative impact on their
self-esteem.

3.2. Addressing
issues related to mental health
19. A Council of Europe/United
Kingdom Parliament seminar held in 2017 highlighted the links between mental
health and justice. The seminar brought together young people, parliamentarians,
NGOs, academics, lawyers and police officers. The recommendations
included the following: improving public awareness; reducing stigma
through campaigns; increasing funding for professional and non-professional
help for young people; improving access to school nurses and psychologists;
developing interdisciplinary services; ensuring that teachers are
trained to recognise signs of mental strain; and ensuring that young
people are listened to and their concerns taken into account, including
when developing laws and policies. At the Council of Europe level,
the Committee for the Prevention of Torture and Inhuman or Degrading
Treatment or Punishment (CPT) should be encouraged to take more
interest in centres for mental health for children. Concerns were
expressed in relation to the number of young people with mental
health problems who enter the justice system, the effect of the
justice system on health and the disproportionate number of young
black men in the justice system. Positive examples included: Austria
(a high level of training for the judiciary), France (a family court
system based on multi-agency co-operation), Iceland (a Children’s
House model – a “one-stop shop” support system), and Nordic States
(increasing use of child-friendly interview techniques, including
video links and written statements). A young participant stated:
“Young people are experts by experience and their stories should
be heard.”

Another seminar for young people
held recently in London has expressed the need for the youth justice
system to be rehabilitative rather than punitive, with a particular
emphasis on mental well-being.

The Spanish interdisciplinary
network for the promotion of mental health and emotional well-being
in the young (PROEM) gives a comprehensive argument for the prioritisation
of mental health and effective interventions).

20. In the United Kingdom, the number of children referred for
mental health treatment by schools has soared by more than a third
in the last three years.

However,
Child and Adolescent Mental Health Services (CAHMS) have to turn
away 23% of children and adolescents. Evidence of the increase in
mental health problems, sometimes referred to as “a crisis”, has
resulted in a number of initiatives. There is a national strategy “No
Health without Mental Health”.

A green
(consultation) paper “Transforming children and young people’s mental
health” was issued in 2017.

The
government has committed an additional £1.4 billion to transform children
and young people’s mental health services. See the Appendix for
information on cost-effectiveness.
4. Sexual
health
21. Encouraging adolescents to
enjoy respectful and satisfying relationships and to protect themselves
not only from unplanned pregnancy, but also from sexually transmitted
infections, requires a combination of accurate information and advice,
services which are welcoming and friendly, and the participation
of young people in identifying their needs and giving advice on
what they find most useful.
22. According to WHO, in 2018, “[s]exual health is a state of
physical, mental and social well-being in relation to sexuality.
It requires a positive and respectful approach to sexuality and
sexual relationships, as well as the possibility of having pleasurable
and safe sexual experiences, free of coercion, discrimination and
violence”.

The terms “sexuality” and “sexuality
education” are adopted in this report rather than the frequently misconstrued
“sex” and “sex education” which have biological connotations and,
to some, implies “having sex”. Educators working with young people
have often found this perception problematic.
4.1. Data
on adolescent sexual activity
23. Data may be questionable, due
to lack of accurate records and incorrect statements by adolescents,
but in Europe, there is reasonably comprehensive data on the sexual
activity of adolescents. For example, there are four teenage births
to women per 1 000 between the ages of 15 and 19 in the Netherlands,
14 in the United Kingdom, 38 in Georgia and 37 in Albania. Sexually
transmitted infections are rising amongst adolescents in European
countries and the increase is higher than in any other group. Condom
use is more frequent than the pill, but the lack of condom use amongst
adolescents leaves them vulnerable to STIs, the rates of which are climbing;
the highest numbers of infections are found among adolescents from
lower and middle income groups.

Whilst advances have
been made globally in the prevention of new HIV infection, progress
has been slow. Globally, HIV/AIDS was the ninth leading cause of
death amongst young people between the ages of 10 and 19 in 2015.

Only 36% of young men and
30% of young women aged 15 to 24 had a good knowledge of how to
prevent HIV according to available data for 2011-2016 in 37 countries.

Adolescents
in Europe are lacking accurate information, and the skills to negotiate
safer sex. They frequently describe their knowledge about sexuality
as “Too little, too late”.
4.2. Addressing
issues related to adolescent sexual health
24. The reasons for early sexual
activity and lack of protection are varied: socio-economic status,
lack of family openness in discussing sexuality and the use of alcohol
or other substances which lower the locus of control.

It is clear that improvements in
awareness and practice can change sexual habits. The UK Teenage Pregnancy
Strategy combines efforts from communities, young people, schools
and services with focus on reducing the high rates of teenage pregnancies.

Between 1992 and 2014, conception
rates fell by 51% with considerable reductions in geographical areas
of high conceptions.

25. Young people should have the right to advice at the start
of their sexual and reproductive lives. However, parents may be
reluctant to engage in such discussions, adolescents may not wish
to discuss sexuality with their parents, and information from friends
or the media might be misleading. Specialist health or education services
are therefore important in providing advice and information.
26. A consensus statement from Public Health England supports
a positive, life course approach involving choices and control as
opposed to the absence of disease or poor outcomes; services that
are inclusive of the population’s needs and responsive to diverse
characteristics; an agreed ethical framework, which takes account
of stigma and shame at all stages of life at an institutional and
individual level; and campaigns that challenge stereotypes and taboo.
27. Young people have made it clear what kind of services they
find most helpful: non-judgmental, confidential, free, and staffed
by sympathetic and knowledgeable staff. One example of such services
is provided by Brook Advisory Centres for young people in nine regions
of the United Kingdom, established over 50 years ago, amidst great
controversy, by the pioneer Helen Brook. These Centres provide comprehensive services
in sexual health for young people up to the age of 24.
4.3. Comprehensive
sexuality education
28. Comprehensive sexuality education
follows the concept of the life course approach to adolescent health. It
advocates structured programmes, which begin with simple information
and discussion about friendship and body parts and move on to more
complex aspects of relationships and sexual behaviour as the child
matures into adolescence and beyond.
29. An overview of sexuality education in the 25 countries of
the WHO European Region concluded that “remarkable progress” in
developing sexuality education has been made since the year 2000.

Other evidence supports
this, but quality and comprehensiveness may not be universal in
the region. Many service providers and educators have struggled
to establish even minimal rights for young people to be provided
with information.
30. UNESCO puts forward the following framework for consideration:
comprehensive sexuality education should cover the full range of
topics (even if they are challenging in some social and cultural
contexts); it should be based on a human rights approach, which
includes gender equality, and should encourage young people to recognise
their own rights, respect the rights of others and advocate for
those whose rights are violated. It may have reference to the overall
well-being of young people whilst impacting the prevention of HIV,
STIs, unintended pregnancy and gender-based violence. It should
provide opportunities to nurture positive values and attitudes toward
sex and relationships and develop life skills to support healthy
choices.

Comprehensive sexuality
education may be included in health education which encompasses
not only the formal school curriculum, but also school ethos and
policies, liaison with parents and communities, and linking with
youth organisations. See the Appendix for information on cost-effectiveness.
5. Obesity
31. Obesity in children and young
people is a relatively new phenomenon, but the problem is global
and has spread at a disturbing rate. It has been called one of the
most serious public health challenges of the 21st century

and
is increasingly affecting low and middle income countries, particularly
in urban settings.
32. The body mass index (BMI) is a person’s weight in kilograms
divided by their height in metres squared. Obesity is defined as
a BMI of 30 and above. Overweight is a BMI of 25 to 29.9.

BMI is measured differently in adults
and children and is evaluated using age and gender specific charts
that take into account the different growth patterns. Weight and
the amount of fat in the body differs for boys and girls and those
levels change as they grow; it is expressed as percentiles. BMI
levels in children and adolescents are expressed relative to other children
of the same age and gender. In adolescence a percentile higher than
95 is considered obese and an 85 to 95 percentile as overweight.

5.1. Data
on obesity
33. Globally, in 2016, the number
of overweight children under five was estimated at over 41 million.
In the WHO Europe region, in 2008, one in three 11-year olds were
overweight; over 50% of both men and women were overweight and 23%
of women and 20% of men were obese. Currently 30% to 70% of men
and women are overweight and 10% to 30% are obese.

Whilst
the European region has achieved great success in improving adolescent
health in recent years, obesity continues to rise in all but a few
countries, with marked disparities. In 10 of the 16 countries and
regions, patterns of social inequality were observed. However, none showed
a significantly higher prevalence of obesity amongst the most affluent
adolescents.

5.2. Influences
on obesity
34. Adolescents become overweight
or obese for a number of reasons, most commonly due to genetic factors,
lack of physical activity, unhealthy eating patterns or a combination
of these factors. In some rare cases, obesity is caused by a medical
condition such as a hormone problem. TV viewing is decreasing across Europe,
but computer usage increased significantly between 2002 and 2014.
Increases in computer use are more evident in girls. The current
guidelines of less than two hours a day of computer or TV usage
is not met by the majority of European adolescents.

Poor
nutrition is the largest factor contributing to poor health, with one
particular cause being the drinking of sugar-laden fizzy soft drinks,
drinks from concentrates, milk drinks, sports and energy drinks
and flavoured waters. Their promotion often targets children and
adolescents. Obesity is more common in lower socioeconomic groups.
Such inequalities are either unchanged or have become greater since
2012. An estimated 27% of all adolescent obesity in Europe in 2014
was attributed to socio-economic differences.
5.3. Consequences
of obesity
35. Most health problems related
to obesity do not become apparent until adulthood. Childhood obesity
is strongly associated with risk factors for cardiovascular disease,
type 2 diabetes, orthopaedic problems and musculoskeletal problems
such as osteoporosis.

If
this trend continues then there will be 88 million people living
with diabetes in 2045 in comparison with 58 million today and the
total health-care costs of diabetes will rise to 175 billion euros
in 2045, not taking into account other indirect costs.

Obesity
could be linked to 12 types of cancer and will overtake smoking
as a leading cause of death within a couple of decades in countries
such as the United Kingdom.

Obese
children are at greater risk of school absence, psychological problems
and social isolation deriving in part from lower self-esteem.

5.4. Addressing
obesity in adolescence
36. Targeted efforts are needed
to break the cycle of obesity. Services should be aimed at adolescents,
to help them make positive changes in health behaviour. Policies
should promote awareness of, and access to, healthy diets and physical
activity,

through
co-ordinated actions of different government departments, communities,
the media and the private sector.

Parental
influence is significant, and needs to be supported. An overall
healthy lifestyle in mothers has an impact on the risk of obesity
in children.

37. Policy actions such as a tax on sugar sweetened drinks, school
food policies, marketing restrictions, food labelling and targets
for the food industry are needed to reduce levels of obesity. Taxes
on sugar, tobacco and alcohol have been suggested as a means of
achieving the Sustainable Development Goals (SDGs) and as part of
a broader public health approach in addressing the commercial determinants
of health.

In
the United Kingdom a regulatory approach was introduced in April
2018: companies manufacturing soft drinks with added sugar have
to pay a levy and there is a higher rate for drinks with higher
levels of sugar. This levy appears to be having a positive effect
as companies are substantially reducing the sugar content in drinks.
The voluntary reduction of sugar in foods was disappointing, with
only a 2% reduction in sugar in the first year. Companies tend to
work around public health concerns to preserve profit margins. Other
areas where legislation could have a positive effect are in agricultural
policy, food marketing and pricing, non-broadcast advertising and sponsorship.
38. The United Kingdom Parliamentary Health Committee recommended
restrictions on advertising and food promotion and giving greater
powers to local authorities to control fast food outlets and billboard advertising.

In 2016, the United
Kingdom set out a plan to combat childhood obesity and built on
this plan in 2018. A summary of actions includes sugar-intake reduction,
calorie reduction, consulting on advertising by introducing before
the end of 2018 a 9 p.m. watershed on television advertising of
high fat and sugar foods. Local trailblazer programmes will be introduced
with local partners to show what works in different localities. See
the Appendix for information on cost-effectiveness.
6. Conclusions
39. Mental health problems among
adolescents are of growing concern across Europe, challenges to
the well-being of adolescents in relation to sexuality are numerous
and obesity rates are growing at a disturbing rate. Meanwhile, it
is in adolescence that behaviours can be changed and foundations
for healthy and fulfilling lives can be laid. Addressing the health
needs of adolescents is imperative, not only for the present generation, but
for the future well-being of populations.
40. Addressing health issues of adolescents has substantial economic
benefits for their societies, including a significant economic impact
on the health system and the wider economy, with implications for
the Europe 2020 Strategy for Growth.
41. Although the amount of research into the consequences of adolescent
behaviours and attitudes is increasing, it is still behind the amount
of research into other age groups. This must be remedied at national and
international levels. It is not clear how many nations in Europe
have a national policy focusing on the needs and potential of adolescents
and the social and economic benefits of directing attention to this
age group.
42. As with other health-related interventions, it is difficult
to isolate the impact of a particular intervention on any health
issue from the determinants of health. It is clear, however, that
tackling these determinants will be key to overcoming poor health.
For example socio-economic status, in particular poverty, inequality
and deprivation, play a dominant role. Economies, which are based
on profit and have few incentives to pay attention to public health
concerns, have a major impact. Media promoting physical perfection
at any cost can be a major influence. Exclusive focus on individual
responsibility is therefore not sufficient, and systemic approaches
need to be developed. States need to formulate approaches to adolescent
health which are human rights based, non-patronising, inclusive,
and collaborative and which counteract stigma or discrimination.
43. Statements and declarations from international bodies are
useful and supportive. Improving adolescent health in the Council
of Europe member States is an important contribution to the United
Nations Sustainable Development Goals.
44. At country level, local initiatives based on needs assessment
and involving local communities are essential in order to deliver
and evaluate the impact of any initiative, and to share best practice.
Health interventions have proved to be most successful and efficient
when they meet the needs of adolescents. Adolescents are the best
experts on their health problems and concerns, and their views must
be taken into account when developing relevant policies and practices.

![]()
![]()
![]() One in five girls in the United Kingdom
self-harm because of worries about their appearance or what other
children have said about their sexual behaviour.
One in five girls in the United Kingdom
self-harm because of worries about their appearance or what other
children have said about their sexual behaviour. ![]()
![]() . Children with better emotional
well-being make more progress in primary schools and are more engaged
in secondary school. This alone suggests a good return for efforts
undertaken in academic settings.
. Children with better emotional
well-being make more progress in primary schools and are more engaged
in secondary school. This alone suggests a good return for efforts
undertaken in academic settings.![]() interventions
for child mental health are listed and analysed and have quantified
costs and benefits. For example, as regards prevention of conduct disorder,
every pound spent would yield £7.83, early intervention in psychosis
would yield £10.27 and suicide prevention would yield £43.99. This
includes costs linked to health-care, police and other emergency
services, loss of productivity due to premature death, as well as
grief and shock experienced by relatives.
interventions
for child mental health are listed and analysed and have quantified
costs and benefits. For example, as regards prevention of conduct disorder,
every pound spent would yield £7.83, early intervention in psychosis
would yield £10.27 and suicide prevention would yield £43.99. This
includes costs linked to health-care, police and other emergency
services, loss of productivity due to premature death, as well as
grief and shock experienced by relatives.![]()
![]() There
is evidence to show cost effectiveness of positive interventions
regarding safeguarding, school readiness, being in education, employment
or training and mental health.
There
is evidence to show cost effectiveness of positive interventions
regarding safeguarding, school readiness, being in education, employment
or training and mental health. ![]()
![]()
![]() two issues
are emphasised: “Strong and mandated central policy, supporting
bold, holistic local action is needed to impact what is arguably the
greatest health challenge of the 21st century …” and “Learning from
joined-up programming emphasises the importance of not only improving
child nutrition, health education and physical activity, … but also
water consumption, access to affordable nutritious food, parent
education … and including improvements in the built environment.”
two issues
are emphasised: “Strong and mandated central policy, supporting
bold, holistic local action is needed to impact what is arguably the
greatest health challenge of the 21st century …” and “Learning from
joined-up programming emphasises the importance of not only improving
child nutrition, health education and physical activity, … but also
water consumption, access to affordable nutritious food, parent
education … and including improvements in the built environment.”![]() The
cost effectiveness of a four-year randomised controlled trial in
a school-based obesity programme in 18 elementary schools saved
US$317 per student balanced against the cost of the intervention.
The
cost effectiveness of a four-year randomised controlled trial in
a school-based obesity programme in 18 elementary schools saved
US$317 per student balanced against the cost of the intervention. ![]()
![]()